Keratoplasty (Corneal transplantation)
The cornea is a transparent membrane that, due to its transparency, allows images to pass through into and enter the eye.
If the cornea loses its transparency, images are no longer focused on the retina; initially, we proceed with drug therapy and, if this does not have decisive effects, we proceed with keratoplasty.
Keratoplasty is a surgical operation that consists in performing a total corneal transplant (or of a part of the cornea), removing its opaque part.
Corneal transplantation can be caused by deep cuts, severe infections corneal dystrophies and keratoconus.
Generally, this surgery is indicated for the purpose of recovering the decline of visual acuity, but it happens that for some conditions it can be used for tectonic purposes. More rarely, this surgery is performed for aesthetic purposes (for example, in cases of disfiguring corneal alterations in the eyes of blind patients).

There are three surgical strategies to perform keratoplasty, and the choice is made according to the type of damage to the. In all keratoplasty operations, the cornea for the receiver comes from the Eye Bank and is accompanied by a certificate attesting its origin and the absence of transmissible corneal diseases.
In the event that the cornea needs to be completely replaced, we proceed with perforating keratoplasty, that is with the removal of the whole corneal tissue and its replacement with a healthy one. If instead, as is the case with keratoconus, the corneal pathology spares one of the layers that compose it, we proceed with anterior or posterior lamellar keratoplasty.
The first method involves removing the first corneal layer, either through manual techniques or the use of the laser, and replacing it with a portion of healthy cornea. Deep lamellar keratoplasty, used for keratoconus, consists in the removal of the deepest part of the cornea, the endothelium (that’s why it is also called endothelial keratoplasty). This surgery is performed under local anaesthesia, either as an outpatient procedure or during hospitalization, and the duration of the recovery period is established by the ophthalmologist in charge.
After surgery, the symptoms most complained of are photophobia, dazzling, diplopia (double vision), and slight pain, but as early as the day after surgery they tend to decrease. Visual recovery is not an immediate effect but takes some time; a certain measurement of visual acuity and of the total recovery of the functions and features of the cornea s performed within 6 months after surgery.
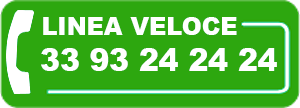
Want to learn more?